Introduction
Governments, policy makers, and health researchers are showcasing ‘digital health’ as the means to achieve universal health coverage (UHC) and to make health-care systems safer, more affordable, and more accessible. Increasingly, they are propagating the idea that they can achieve ‘citizen‐centric care’, improved access, universal health coverage, and inclusiveness by ‘leveraging the power of digital technologies’[1] (Sharma et al 2023; Kodali and Das 2021; WHO 2016).
What exactly is ‘digital health’?
The term ‘digital health’ is quite broad. It includes a range of tools and services that use information and communication technologies[2] (ICTs) in medicine and healthcare.
Such technologies can be used to improve prevention, diagnosis, treatment, monitoring and management of health problems. For example, data regarding the health of patients and the care they are receiving can be collected, shared and analysed using phones, computers and other devices. Medical records can be stored in electronic form. Big data analytics, advanced computing and artificial intelligence may be applied to these data. All these technologies and practices could enable better understanding of the state of public health, better diagnosis, and more efficient care.
There are other senses in which the term ‘digital health’ is used. One such is telehealth or telemedicine, that is, when a doctor (or other healthcare provider) and a patient are separated by distance, and the former guides the latter using electronic communication (e.g., phone or computer). Finally, the term may also be used for ‘mobile health’ (mHealth) – the use of various types of personal mobile devices to monitor vital signs, track activity and access medical care and advice.[3]
In this commentary, we focus on the National Digital Health Mission of India (NDHM). The NDHM, announced in 2020, claimed it would deploy digital technologies to achieve the goals of the National Health Policy — universality, ‘citizen-centricity’, quality of care and accountability. It also claimed it would make the delivery of healthcare more efficient and effective.
‘Digital Health’ in India since the 1990s
TeleMedicine
The Government began extending telemedicine services to rural areas in the late 1990s.[4] As recounted by one of those involved in the introduction of telemedicine services in the country (Ganapathy n.d., Ganapathy 2020), this project from its inception involved the private corporate sector (Apollo Hospitals) and non-governmental organisations (NGOs).[5]
Drawing on India’s large medical and IT manpower, various Government and private telemedicine solution providers began extending telemedicine services within the country. Within about a decade several states had implemented different models of telemedicine, with varied levels of success. Not only did the Government implement various national-level projects, but it promoted telemedicine services in other South Asian and African countries.
Whether funded and operated by the Government, or Government-funded and operated by private parties (public–private partnerships), most telemedicine networks in India function in a hub‑and‑spoke model. The hub is typically a medical centre providing super-speciality care, such as a medical college hospital, and the spokes are facilities such as district hospitals (DHs), community health centres, primary health centres, and sub-centres (now renamed ‘health and wellness centres’, or HWCs). (Telemedicine consultations are also provided by private platforms such as Practo and 1 mg.[6])
Electronic Health Information Systems
There are, no doubt, potential benefits of digitisation. By collecting and analysing data regarding the performance of public health systems, we can improve their management, decision-making and performance (Gowda et al 2022; Zodpey et al 2016), and digitisation can help this process.
Take, for example, the Comprehensive Rural Health Services Project Ballabgarh (CRHSP), run by the All India Institute of Medical Sciences (AIIMS), New Delhi. The CRHSP was started in 1965 with the objective of demonstrating a model healthcare delivery system, and for training medical students.(Its Intensive Field Practice Area in Ballabgarh, Haryana, comprises 28 villages, catering to a population of over 85,000 in 2008.)
The CRHSP’s computerised Health Management Information System (HMIS) was set up in 1988, and has step by step extended its reach, making it more and more comprehensive.[7] By 2011 the CRHSP was gathering data on the performance of individual health facilities, down to the level of the Primary Health Centre, to enable micro-level planning. Covering 747 districts and 2.17 lakh facilities, it is one of the largest such Management Information Systems in the world. However, the quality and usability of the data collected by the HMIS of CRHSP data remains an area of concern. Lack of adequate training of health workers, including data entry operators and MIS officials, results in poor data quality. In addition, there is poor coverage of, and reporting of information from, private hospitals.
Adoption of electronic health records (EHR) in India is reported to be low, with a few private corporate hospitals having their own EHR systems with little or no interoperability. Electronic medical records (EMRs) are rarely exchanged between hospitals. Digitisation at AIIMS Delhi was initiated in 2012, as a result of which large amounts of data have been accumulated, which can be expected to increase over time (Gowda et al 2022).
National Digital Health Mission: private corporate sector present at the conception
As several such initiatives and policy measures were taken over the past two and a half decades, infrastructure became increasingly available, and operational models were set up. All this laid the foundations for the launch of the National Digital Health Mission, National Digital Health Blueprint and Ayushman Bharat Digital Mission through 2020-21 (Agarwal et al 2020).
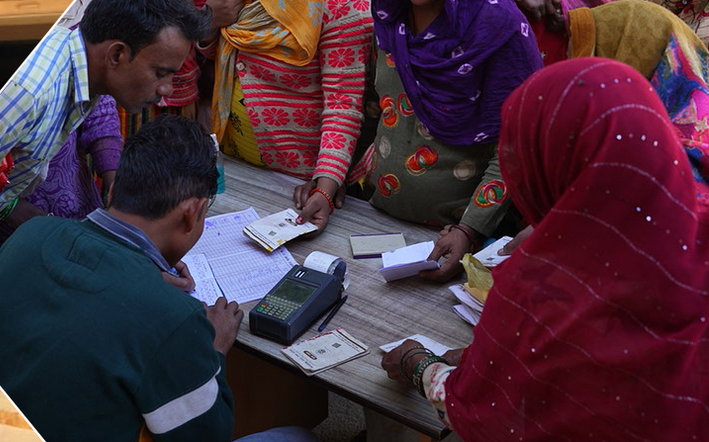
Additionally, with the policies of economic liberalisation since the 1990s and the promotion of public-private partnerships in various fields, the Government increasingly turned to the use of information and communications technologies for development/social welfare activities. The Government brought in the Information Technology Act 2000, and the erstwhile Planning Commission set up working groups on designing digital technology for welfare programmes. The year 2008 saw the first use of digital authentication in health, with chip-enabled smartcards in the Union government health insurance scheme, Rashtriya Swasthya Bima Yojana (RSBY). The latter is seen as the beginning of digital healthcare in India (Al Dahdah and Mishra 2023, 2020).
RSBY was scaled up in 2018 with some changes, and renamed later as Pradhan Mantri Jan Aarogya Yojana (PM-JAY). PMJAY is paperless, and functions through an IT system. “Creating the world’s best health assurance programme on an efficient and technologically robust ecosystem” is the stated Mission of PMJAY (Government of India 2023 p 6). PMJAY also continues the emphasis on pro-private sector measures initiated in the 1990s as part of the health sector ‘reforms’ promoted by World Bank and other influential sections in health policy making, and the recommendations of the 2010 High Level Expert Group (HLEG) on UHC. These measures include ‘strategic purchasing’, contracting from the private sector, and expansion of the private sector and market-oriented solutions (Srivastava et al 2023; Chakravarthi 2019).
The Government, and more importantly, the private corporate sector, cannot ‘leverage’ digital technology for health when the relevant data are fragmented, scattered around various entities, and not standardised. In order to build a single ‘ecosystem’, the Government is on a drive to standardise and centralise all health data. For this it drew up a National Digital Health Blueprint (NHDB) in 2019.
The private corporate sector was present at the conception of the NDHB. The Blueprint incorporates recommendations of the India Digital Health Net (IDHN), a research and policy collaboration of the Lakshmi Mittal and Family South Asia Institute at Harvard University, USA. IDHN comprises medical practitioners, technical and legal experts, and policy makers from India and the USA. Since 2016 the IDHN has been focussed on the development of a digitally-enabled health exchange ecosystem,[8] which has been adopted by the NDHB.
To implement the NDHB, the Government has set up the National Digital Health Mission. After integrating the data available in various locations and institutions, the NDHM is meant to set up digital records, registries and a framework allowing different parties to smoothly access, share and use health data.[9] The NDHM is responsible for the following services:
— a single, secure health ID to all citizens;
— personal health records;
— a single (national) health portal;
— a health app store;
— specialised services for remote areas/disadvantaged groups;
— an NDHM call centre;
— online appointments, digital referrals and consultations, clinical decision support, and case transfers;
— an e-prescription service;
— digital child health;
— a national “opt-out” (for privacy);
— an open platform to access emergency services;
— technology for ‘practitioner transformation’ (sic);
— case transfers;
— digital pharmacy and pharmacy supply chain;
— hospital digitisation; and
— digital diagnostics.
The National Health Authority (NHA), an autonomous body under the Ministry of Health & Family Welfare set up to implement the PMJAY, is also responsible for the implementation of the NDHM.
It is evident that the private sector will play a major role in the NDHM, on the plea that it will bring in funds. Noting that the capital cost for development, human resources and operating costs formed the major cost components of NDHM, the Government envisioned that the necessary resources would be raised from private sector and market players, such as med tech companies, NGOs and foundations working in health, to build up the registries, health ID, electronic health records, etc (Government of India 2019 p 46).
Another important component is the NDHM Sandbox (NS), a recommendation of the India Digital Health Net, submitted to the Ministry of Health and Family Welfare in 2019. Just as a real sandbox is a protected space in which a child can safely play on its own, a tech ‘sandbox’ is a protected environment in which new software can be tested without harming the wider system. In the sphere of digital health, these sandboxes are
controlled testing environments within which existing regulations may be temporarily relaxed to allow experimentation for novel technologies. They provide the enabling conditions that administrators need in order to test new solutions in subsets of populations in a responsible, controlled, and monitored real-world environment, before mandating change at scale. [10]
Through the NS, the Government is providing private healthcare/health tech firms access to a controlled environment to carry out live testing of their IT products or innovations. The Government claims that the NS will allow the Mission, the innovators, and the healthcare service providers (as potential deployers of the technology) to conduct field tests of products integrated with NDHM building blocks, while carefully monitoring and containing their risks.[11] It claims that this will enable responsible innovation in health tech services, promote efficiency and bring benefit to consumers. [12]
In other words, the NS is about providing software providers, hospitals, labs, healthcare aggregators, and health tech companies a ready, organised space to test their products/innovations without a large-scale roll-out. For instance, the SAMRIDH scheme (Sustainable Access to Markets and Resources for Innovative Delivery of Healthcare – explained later), a platform set up by the Government along with several private organisations to raise funds for expansion of private healthcare sector and for healthcare technology innovations, has a collaboration with NHA-NDHM and access to PMJAY’s network of 24,500 healthcare facilities, to test and mainstream their innovations[13] (NITI et al 2022).
Present state of affairs
Telemedicine
The National Telemedicine Service in India is now delivered under Ayushman Bharat Scheme of Government of India. The ‘eSanjeevani AB-HWC’, is a telemedicine platform through which a doctor at the spoke (a Health and Wellness Centre in a rural area) can consult a doctor/specialist at the hub (say, an urban hospital) via video conferencing. The “eSanjeevani OPD – Stay Home OPD”, is an online OPD service, whereby a patient can consult a doctor at the hub, via a doctor at the Health and Wellness Centre. At the end of the consultation, Sanjeevani AB-HWC generates an e-prescription.
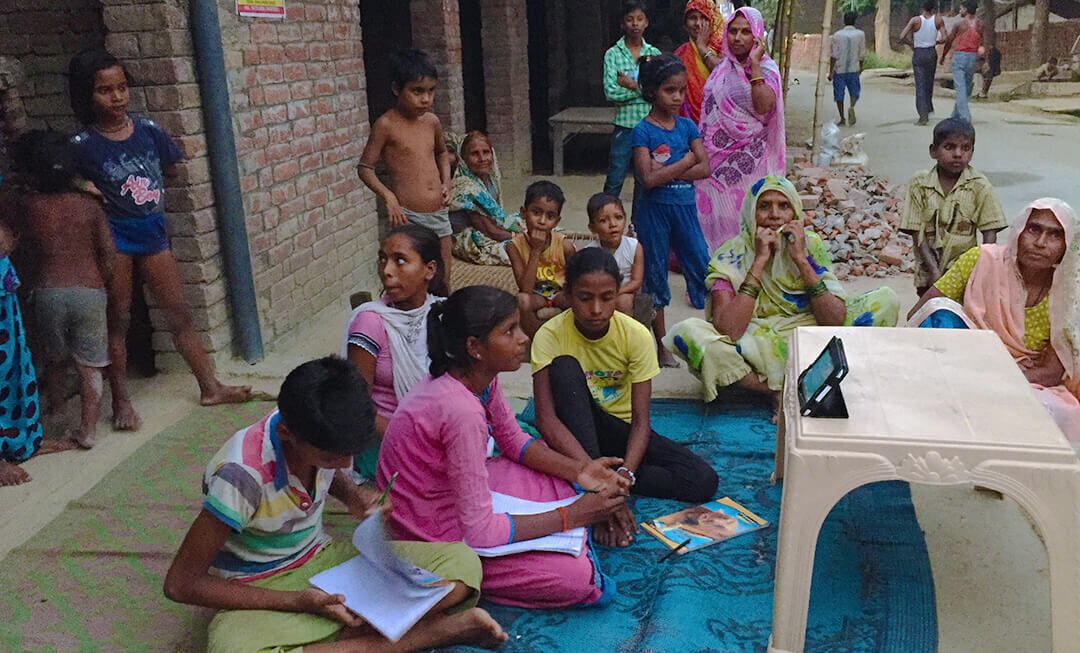
A big challenge in delivering online consultations via eSanjeevani OPD has been the shortage of doctors and specialists, leading to long waiting times, especially for consulting specialists. Access was another problem: the eSanjeevani platform is solely video-based, and requires the patient to have a smartphone or laptop with an internet connection. Hence those with no access to internet connectivity, or those without a smartphone, cannot use this telemedicine facility. Moreover, patients are required to fill the registration form (available only in English) online. All such factors end up depriving the most vulnerable segment of the population of access to the remote consultation services. This is a situation of digital exclusion in healthcare.
Other problems included issues of poor connectivity, long waiting times, and the absence of scope for queries/questions etc (Bajpai and Wadhwa 2021). There were also problems of inadequate training of staff and shortage of staff, heavy workload, poor network connection, and lack of awareness among people about availability of such services at the health centre (Kanwar et al 2023). There have also been reports of incidents of sexual harassment of women doctors on Indian telemedicine platforms that offer consultations with doctors (Khanduja, Goli, and Singh 2021), with ‘patients’ masturbating or making lewd conversation in the guise of seeking consultation. Instead of informing the police of such incidents, the platforms kept it under wraps and implemented additional measures to prevent such incidents, without much success. Such incidents contributed to the unavailability of female doctors for consultation on these online platforms.
Electronic Health Records/Electronic Medical Records
According to Mitra et al (2023), India has crossed the first stage of digitalisation, in which most paper-based information is captured in electronic forms, including imaging data in x-rays and CT films. India is now into the second stage of digitalisation, in which electronic health and medical records are being collected, and telemedicine consultations are taking place.
To achieve complete digitalisation, healthcare facilities (both public and private) will have to adopt digital workflows, i.e. the automation of processes. The final stage of the digital evolution is digital transformation, where the good quality data from the health system is ‘leveraged’.
However, much remains to be done to achieve this, due to the state of health information data in India. There are problems with the quality, completeness, and reliability of the data, and health care professionals are not trained on the importance of data and its use in the decision-making process. Barely five per cent of all healthcare data is collected in India, out of which only a tiny fraction is being used for public health decision-making. All the four stages of healthcare analytics, namely, data generation, data extraction, analysis, visualisation and reporting need to be worked on, for it to be useful for decision-making. The stage of data generation being the very foundation is critical, as it provides data in digital format, which enables further analyses and visualisation.
A study of the health information system (HIS) at AIIMS Delhi, conducted between 2016 and 2018, gives an idea of the challenges to be overcome in use of such a system and of electronic health records even within a single institution (Gowda et al 2022). Some tasks were working well, such as appointment booking, receiving or transferring patients between wards and discharging patients, ordering tests and receiving results. However, several problems in the implementation of the system were highlighted. There was no unified login portal, and each user had to access multiple login portals, making the whole process tedious and time consuming. There was no sharing of data between applications meant for different processes. There was redundancy, with the users having to enter the same data in different applications, due to lack of interoperability. Lack of structural interoperability was also impairing process interoperability. Implementation of the HIS entailed new tasks for them, which meant the overall workload had increased. Paperwork continued or had increased despite implementation of the system, contributing to increased workload. Information in the system was not always updated; the system was not stable and crashed often; and there was inadequate staff for implementation of the system. Problems reported from other countries were also seen in this study, such as burn-out among clinicians, lack of a human touch, excessive screen-time, and lack of overall work satisfaction and fulfilment among clinicians due to compulsory implementation of electronic health records.
The authors of the study point out that the basis/rules used for the development of computer systems are different from the actual processes of clinical work. As a result, “The processes and systems are forced to fit into the software rather than other way round”, giving rise to a rigidity that made it difficult for doctors using these systems.
A ransomware attack in November 2022 on the servers of AIIMS Delhi crippled patient registration, online appointments, diagnostic report generation, and billing, as well as administrative systems such as salary disbursal and drug procurement (Malhotra 2023). For almost two weeks, these services were managed manually, leading to long queues and increased waiting times. The personal data of more than 30 million patients and healthcare workers were compromised. Investigations revealed that there were several cybersecurity lapses, such as the firewall not being configured properly and the lack of safeguard switches at several points. These had been brought to the notice of the hospital authorities (Singh 2022). Several private hospitals also have had their systems hacked into, compromising the records of a few lakhs of patients. India’s health sector is the second most targeted for cyberattacks in the world, accounting for 7.7 per cent of all attacks on healthcare institutions in 2021 (the United States tops with 28 per cent), according to cybersecurity intelligence reports (cited in Malhotra 2023). Such incidents raise grave concerns about the state of cybersecurity in India and protection of patients’ health information in digital systems.
Concerns about NDHM digitisation
Will NDHM improve access to healthcare?
The Indian Medical Association (IMA), the largest organisation of allopathic doctors, has expressed several concerns about the NDHM. According to it,
India still lacked adequate infrastructure and trained personnel for healthcare services; primary care had lost focus and the wellness centres were yet to have impact; strategic purchasing through PMJAY was not having as much impact due to lack of adequate fund allocation and non-empanelment of tertiary care hospitals due to unrealistic package rates. The priority should be strengthening of public health infrastructure and human resources, as well as addressing the social determinants of health. Funding for such an ambitious plan was not clearly spelt out; any diversion of funds from NHM would further jeopardise the public funded health care, especially primary care.[14]
Privacy was another area of concern pointed out by the IMA, as privacy protection laws in India are weak and practically non-existent. It has pointed out that consent in digital platform in a country where literacy is low is a cause of concern; and the consent mechanism provided in the document was inadequate to address the concern. [15] According to the IMA Secretary, “We are not sure how the programme will improve access to health care. If the idea is to collect data, there are initiatives such as the national health survey, which does a great job. As far as patients are concerned, 99 percent of them don’t leave their district. In that sense, how does interoperability help?” (Balachandran 2020).
Whether it be for telemedicine or for hospital information systems or electronic health records, substantial infrastructure has to be created in most public hospitals, in terms of infrastructure, computer hardware, software, connectivity and cybersecurity. Whereas, most of the public healthcare facilities in India continue to be chronically under-resourced, under-staffed, under-funded, with the rural/peripheral health centres the worst-off in several states. Telemedicine has not been able to address shortage of doctors; rather, it suffers from the very same problem of shortage which it is expected to remedy. Clearly the goal of drawing in private providers to address the chronic shortage of specialists is also not satisfactorily materialising.
Another issue is that of digital inequalities and limited digital literacy. Based upon data of the Telecom Regulatory Authority of India, it has been estimated that, as of March 2022, just 60 percent of India had internet access. Importantly, almost 100 percent of urban population had access, as against 37 percent of the rural population. Internet access was concentrated in the top 30 cities. Further, 57.1 per cent of the male population used the internet, as against only 33.3 per cent of the female population (Dhole 2022). Not much is known about use of the internet in India. As mentioned above, studies have pointed out that access to telemedicine is impacted by poor connectivity and inability to follow instructions in English to register online.
Internet access on its own does not ensure that users are able to use all the digital tools, including those for accessing healthcare. Let alone individuals, analysis of the NSSO 73rd round (2015–16) survey data showed that only 40 per cent and 34 per cent of private unincorporated hospitals reported use of computers and internet, respectively, in the previous 365 days; and only 33 percent of unincorporated hospitals reported use of both computers and internet in the preceding 365 days (Chaudhari and Datta 2020).
For those who do not have the skills and access, imposition of a digital mode can increase their reliance on others to assist them, making them vulnerable to fraud and manipulation. In addition, it can increase the disparities between those who have skills and access to digital tools and those who do not, and thereby increase existing health disparities. As rightly pointed out by others, digital access is becoming another social determinant of health (Sieck et al 2021), shaping access to other social determinants of health, including access to hospital services.
Looking beyond design and implementation issues of NDHM – convergence of technology-big data-business in healthcare
Beyond the issues and concerns outlined above, it is important to also keep in view other associated developments, as delineated below, which indicate that there is much more to the NDHM and this thrust to create a digital health ecosystem.
What is clear is that the NDHM and what it proposes to do – deployment of digital technologies in health services, the setting up of a digital infrastructure for health information, the assignment of digital health IDs – are not really as novel or revolutionary as the current fanfare and hype around them seek to convey.
Two objectives, however, stand out: (i) the centralisation of all health data, whether they be personal health records or systems information, and the creation of a dedicated national level authority for this purpose through the national level health insurance scheme; (ii) the provision of a platform for testing of IT products for the creation and the sharing of such centralised digital health information system, through the Sandbox mechanism, as mentioned earlier.
The questions posed by the IMA remain pertinent in this scenario. How, if at all, will the centralisation and portability of all the information address the well-known chronic health systems problems such as underfunding and shortage of human resources? What are the lessons from the use of ICTs in the existing state health insurance schemes? How are the financial-material-human resources for digitisation going to be provided? Can and will the NDHM address the known problems and barriers in achieving UHC? Is this the only way to digitise health information? What will the impact of this testing/piloting of digital innovations be on the access of the people to the medical care under PMJAY – steps such as beneficiary registration-enrolment-approval of treatment? The CAG audit of PMJAY has already pointed out the mismatch problems in the registration and enrolment (Government of India 2023).
“Big Data Meets Public Health”[16]
The NDHM and its thrust on creating mechanisms for standardising and sharing patient health information assume particular significance in the present context, as reflected in the following observation:
In healthcare, data mining is becoming increasingly popular, if not increasingly essential (Koh and Tan 2005).
The organisation of medical care has become increasingly technology-intensive over the past century, and such medical care in turn has been equated to individual and public health. Against this background, it is not surprising that now ‘big data analytics’ is being promoted as having much promise for public health:
There is much excitement globally about the power of big data, artificial intelligence and machine learning in reshaping medicine and health care delivery. However, the potential of these promising sciences can only be harnessed with reliable and timely data. A federated PHR (patient health records) in India will provide unprecedented amounts of health data; among them may lie answers to our well-being and happiness (Balsari et al 2018).
An influential section of public health researchers and practitioners claim ‘big data’ has the potential to benefit medical research; provide insights into the causes and outcomes of disease; design better drug targets for precision medicine; enhance disease prediction and prevention (Khoury and Ioannidis 2014); improve patient care and provider satisfaction; reduce healthcare costs; empower patients (Balsari et al 2018; Wyber et al 2015); and enable digital public health surveillance though DDD – digital disease detection or digital epidemiology (Vayena et al 2015).
Entrepreneurs see potential in monetising the health data. They see data mining applications as promising benefits to the healthcare industry, in activities such as helping insurers detect fraud and abuse; evaluation of treatment effectiveness; management of healthcare; and customer relationship management (Koh and Tan 2005). Not surprisingly, big and powerful IT companies, such as Google, Apple, and Amazon, are reported to be “wading into health care” by trying to play to their strengths (Finley 2018).
Healthcare data mining, particularly in India, has been limited by the lack of availability of clean healthcare data. The raw information/inputs for data mining currently exist in different settings and systems: with the public health administration; in different public and private hospitals and laboratories; with insurers and pharmacists; and with individuals themselves, in their mobile devices. Such data have to be collected, standardised, and integrated before data mining can be done. There have to be mechanisms by which data can be better captured, stored, prepared, shared across organisations, and mined. A large portion of health data collected also remains inaccessible due to valid concerns over confidentiality and privacy, risk-averse hospital policies, prohibitive costs of the change, and inertia among the concerned sections (Balsari et al 2018).
While India has substantial informational technology resources and infrastructure, mobile phone penetration, cloud computing, and financial technology, the digital health ecosystem is comparatively less developed. The lack of a significant insurance player in the market, which could have been used as a vehicle to promote adoption of electronic health records through the billing requirements of payers and providers, is seen as one factor for this situation (Balsari et al 2018).
The Pradhan Mantri Jan Aarogya Yojana of 2018, with its “urgent need for a technological backbone” (Balsari et al 2018) for implementation, changed this scenario, and became the impetus for the NDHM. Even though the NDHM talks of a digital health ecosystem, its genesis and design are more in alignment with the PMJAY, and it is to be also implemented by the same National Health Authority. This suggests that it will largely cater to digitisation requirements of this insurance scheme, and streamline all the information to enable big data analytics.
NDHM as providing ‘digital commons’ and economic opportunities
The private healthcare sector in India has an influential, corporatised segment, which is actively involved in health-policy making (Chakravarthi et al 2023). The response of the industry to the NDHM reveals an important facet and goal of the NDHM. According to the CEO of the National Health Authority and PMJAY, the Natonal Digital Health Blueprint had opened a range of market opportunities for all stakeholders (FICCI and BCG 2020). Industry associations claim that the adoption of a health open digital ecosystem (ODE) can have a transformative impact on India’s public health system, and create immense economic and market value.
A report prepared by the Boston Consulting Group (BCG) and FICCI describes how the NDHM will change the healthcare market dynamics, and unlock multiple economic opportunities for all stakeholders. New players will emerge, and business models will undergo significant shifts; a new class of intermediaries will emerge to build the very foundation of the digital infrastructure, such as health facility verifiers, consent managers, and health locker providers. Health tech startups stand to become profitable; similarly, hospitals also stand to benefit in several ways with the availability of such a digital platform (FICCI and BCG 2020). Among the suggestions of this report is that patients stand to benefit the most from the electronic storage of their medical records and hence should finance this digitisation; so they should be charged a nominal fee for providing a digital record, through which providers can partially recover the cost of upgrading their digital capabilities and become a part of the NDHB federated framework.
What we see is that while, on one hand, the Government is promoting PMJAY and NDHM as the means to universal health care, at the same time, it is also showcasing the NDHM as well as the healthcare sector itself as an attractive business opportunity (Sarwal et al 2021), as well as furthering ways of raising private capital for such private investments (NITI Aayog and SAMRIDH 2022).
Grand alliance of public-global-business actors in health policy-making and implementation
A study of the genesis of PMJAY found that personnel from international and bilateral/multilateral organisations, such as the Bill and Melinda Gates Foundation (BMGF), Gesellschaft für Internationale Zusammenarbeit GmbH (GIZ, the German development agency), the World Bank, and the WHO had played both policy advisory roles (through high-ranking officials) and techno-managerial roles (through consultants placed in middle-management positions within the Government) in setting the agenda and the design of the PMJAY. In addition, business consulting organisations such as IQVIA and PriceWaterhouseCoopers were also involved in the design stage. Civil society and academia were not involved in the process.
While the Gates Foundation had no direct role, it facilitated dialogue between all other stakeholders by hosting meetings, and funded the activities of GIZ and the World Bank through grants (Srivastava et al 2023). Influential financial institutions such as the World Bank and private foundations such as the Gates Foundation are known to provide financial and technical support to IT systems that extend use of biometric cards in the health field (Ecks 2018).
In November 2019 BMGF and the Ministry of Health and Family Welfare signed a Memorandum of Cooperation for co-operation in the field of health, which was approved in January 2020 by the Union Cabinet chaired by the Prime Minister.[17] As per this memorandum, BMGF will work closely with the Government and provide technical, management and programme design support through its grantees and other partners, for key health initiatives and health system strengthening, including aspects such as digital health, budget utilisation, management of human resources for health, strengthening supply chains and monitoring systems.[18] BMGF is known to advocate digital health solutions, and has engaged international experts in digital health to help design a digital health platform under the MoHFW, as they felt that this would be strategic for any future scheme (Srivastava et al 2023). It has given a large number of grants in India, including to Access Health International Inc., to strengthen the institutional capacity (design and operations) of the PMJAY health insurance scheme in five states of India.[19]
A recent study found many contracted resources, ‘implementation support agencies’ and resources provided to the Government through ‘development partner organisations’, as ‘technical support’ in implementing PMJAY at the state and district levels. For instance, the implementation of PMJAY in U.P. had four implementation support agencies and technical resource persons positioned within the state health agency through ‘development partners’, who provided support on multiple functions, including key functions such as processing treatment pre-authorisation requests and provider claims (Furtado et al 2022). Such engagement of outsourced agencies and development organisations raises concerns about institution building, and the ability of the system to develop and retain its own expertise for long-term sustainability in implementing such schemes.
Such involvement of a range of international institutions, including business and private foundations, in policy making and implementation in health sector, is not an isolated instance. Rather, it represents the reality today, of “transnational expert communities working on research, policy and advocacy within organisations located in centres of global power, although their work is focused on the poorest countries” (Storeng 2014). In the name of ‘development co-operation’, ‘technical co-operation’, ‘global public private partnerships’, ‘global health governance’ and so on, such mechanisms function within governmental bodies. They perpetuate notions of paternalism and dominance of professional experts, particularly from the industrialised countries of the Global North, as captured by this view: “In low- and middle-income countries, the shepherding of the transition from paper records to petabytes of digital storage provides another opportunity for global health institutions to offer useful governance” (Wyber et al 2015). More often than not, this expertise in governance is about ‘leveraging private finances for development’ and ‘unlocking the transformative potential of the private sector’. Under these labels, governments accommodate and promote private business – a phenomenon known as the financialisation of healthcare (Hunter and Murray 2019).
This convergence in health, through measures such as NDHM, of private business interests from digital technology and finance, raises grave concerns regarding how the data collected is going to be used, by whom, and to what ends. Will it genuinely serve public health interests, or is there more to it than the rhetoric of UHC?
Will more advanced technology and more data mean improved access and better health?
A report by the United Nations on the opportunities and challenges of using big data for development notes that “it is important to recognize that big data and real-time analytics are no modern panacea for age-old development challenges” (United Nations 2012); that, “application of these approaches to development raises great expectations, as well as questions and concerns, chief of which is the analytical value – and thus ultimately the policy relevance – of big data to address development challenges.”
Will this NDHM deliver on its promise – of improved access, quality care, and all such rosy projections about health and healthcare? Well, have the earlier, similarly promoted, technology advancements in medicine, in diagnostics-surgery-therapy-prevention delivered on the promise of improved health, health equity, quality care, and health for all? As a corollary, how has health of populations improved historically? How have countries, rich ones as in Europe and poor ones like Cuba, managed to improve the health of their populations, achieve health equity and universal health care (and not simply universal health coverage), and that too without the most advanced technologies?
The history of public health and medicine indicates that technology, or economic growth for that matter, by themselves have not led to the vast improvements in health seen in many countries. In the highly unequal society that we are, digital technologies would benefit the affluent sections that have the wherewithal, the resources and ability to access and understand the technology to be able to give consent to use of their personal health data; some other sections would serve as guinea pigs in the trials and piloting of innovations to put in place this complex digital health ecosystem and could get excluded or their access to healthcare could be affected; large sections may remain untouched by this digital ecosystem. Such differences in access to healthcare do not qualify to be called Health for All, and are not what equity and universal, comprehensive health care is about.
The ongoing inroads into health of digital technology and the ways in which it is happening, through NDHM and the variety of assemblage of public and private actors, can be viewed as the latest chapter in the now nearly hundred-year-old discourse and vigorous contestations on the role of technology in health, on what protects and improves public health.
These developments are a reflection and manifestation of the further entrenchment of the view of technology as a solution to the vast inequities in health status and as vast problems in the healthcare sector, a view which has been on the ascendance in the past few decades, coinciding with the rise of neo-liberal policies. In other words, it is an extension of the “disquieting trends in modern medicine and public health – of privatised health economies, of the growth of techno-optimism, philanthro-capitalism, global health’s neo-imperialist tendencies, of the importance of political determinants of health…” (Horton 2017).
We are far from the days of WHO’s 1978 Alma Ata “Declaration on Comprehensive Primary Health Care and Health for All by 2000” and its vision of a New International Economic Order and of appropriate technology.[20] Let alone Alma Ata, it is as if even the WHO’s more recent Commission on Social Determinants of Health (CSDH) and its analysis of ‘social injustice killing people on a grand scale’ (CSDH 2008) do not exist. It is as if public health and UHC were only about technology, and digital technology is the way to UHC. It is as if universal health care, or even universal health coverage, cannot be achieved by other means, or have not been achieved in several parts of the world well before digital technologies became available.
NDHM, in its vision, conception and design, fits into what is being called “the ‘Gates approach’ to global health, an increasingly powerful business-oriented, technology-focused public health ideology, propagated by Bill Gates and his foundation” (Storeng 2014, p871). It seems that through NDHM it is ‘UHC’ that is being leveraged in the interests of the makers and owners of (digital) technology and capital.
Notes
- https://nha.gov.in/NDHM.html ↑
- ICT is an inclusive term, covering all communication equipment or application software: for example, radio, television, mobile phone, computer, network hardware and software, and satellite system, as well as various services and application software related to it, such as video conference and distance learning. The importance of ICTs is not the technology as such, but its enabling function in facilitating enhanced access to information and communication across large distances (Shao et al 2022) ↑
- This article does not discuss ‘mobile health’ (mHealth), i.e., the use of personal mobile devices with specialised software/applications to access medical care, advice and related health information; monitor blood pressure; record blood sugars; ensure compliance with medications; track the amount of physical activity; and so on. Such mHealth tools are becoming popular among the affluent sections. However, there are concerns about them, such as the inadequate clinical validation of mHealth apps, inadequate information among doctors to be able to prescribe or use such apps, and unaddressed privacy, confidentiality and security issues (Bhavnani et al 2016). mHealth is being promoted in mental health (Pillutla 2023) and also among field level health workers such as ASHAs (Accreditated Social Health Activists) and ANMs (Auxiliary Nurse Midwife) for identifying and tracking children and pregnant women, and collecting and processing health data (Prinja et al 2018). ↑
- These services began with the deployment of a SATCOM-based telemedicine network across the country involving the Indian Space Research Organization, Ministry of Health and Family Welfare, Department of Information Technology, Ministry of Communications and Information Technology (IT), various state governments, and several leading technical and medical institutions. The Department of Information Technology defined the Standards for Telemedicine Systems, and the Ministry of Health & Family Welfare constituted the National Telemedicine Task Force. ↑
- A first-hand chronological account by a medical professional associated with telemedicine narrates the beginnings (Ganapathy n.d; Ganapathy 2020). In late 1996, a pilot proposal on telemedicine was presented to Dr Prathap Reddy of Apollo Hospitals by Prof. Ganapathy (past President, Neurological Society of India and Telemedicine Society of India) and Prof. Srivathsan (of IIT Kanpur). In March 2000 the first telemedicine service was started by Apollo Hospitals between its tertiary facility in Hyderabad and its secondary level facility in Aragonda village, Chittoor district, erstwhile Andhra Pradesh. Apollo Health Enterprises then went on to establish, in 2001, the Apollo Telemedicine Networking Foundation (ATNF) as a not-for-profit company, and in 2010 it set up the Apollo Telehealth Services Private Ltd. In 2009 the Indian Ministry of External Affairs initiated the Pan Africa e-Network project for teleconsultations, with active participation of the ATNF. In 2014 promotion of e-literacy in rural India was initiated by the MS Swaminathan Research Foundation through internet enabled Village Resource Centers (Ganapathy n.d.). ↑
- Telemedicine consultations provided by private platforms such as Practo and 1mg include online consultations, drug delivery, appointment services, health check-ups, hospital referrals, second opinions, inpatient arrangements, and domestic/overseas medical services. ↑
- This HMIS has undergone evolution and is currently in its third version which uses generic and open source software (Krishnan et al 2010). A web-based Monitoring Information System and portal, the Health Management Information System (HMIS), conceived and developed by the Statistics Wing of the Ministry of Health & Family Welfare, was launched in October 2008. It started with consolidating district-level information across the country; from 2011 it began capturing performance data of individual health facilities, to enable micro-level planning. Data related to service delivery and infrastructure/human resources is captured in the HMIS on a monthly basis. Its features include: unique formats for different level facilities; data on around 70 data items at the Health Sub-Centre (HSC) level, 117 data items at the Primary Health Centre (PHC) level, and 137 items at the community health centre (CHC), sub-district hospital (SDH) and district hospital (DH) level; offline and online data uploading facility; the capturing of performance related monthly data; provision for uploading infrastructure data such as human resources, clinical facilities, medicines, etc. on an annual basis. Data are made available in the public domain, and customised reports are prepared based on service delivery, infrastructure and survey data (Srivastava 2015). With further improvements, Health Management Information System 2.0 was launched in 2020, as a step towards digital transformation of health services delivery in the country. As of March 2022, around 747 districts and around 2.17 lakh health facilities were reported to be mapped and reporting through the HMIS Portal. (https://main.mohfw.gov.in/sites/default/files/HMIS%20Brief.pdf last accessed 30.12.2023) ↑
- https://mittalsouthasiainstitute.harvard.edu/india-digital-health-net/ ↑
- The NDHM is to be the technology arm of India’s health sector, focussing primarily on the core technical services it shall provide to various organisations, public, private, and NGO, comprising the National Digital Health Ecosystem (NDHE). Its stated functions are: to provide the technology platform for collection of core health data from the providers and patients; to provide a platform for the interoperability of health care data through a unique identifier for the provider and patient across the health system; and to improve the quality of health data collection, storage and dissemination for purposes of research and policy decisions. (Government of India 2019) ↑
- https://mittalsouthasiainstitute.harvard.edu/india-digital-health-net/ ↑
- According to the NDHB, the NS is “a framework that will allow technologies or products to be tested in the contained environment in compliance with NDHM standards and judge the consumer and market reactions to the same. This will help organizations intending to be a part of the National Digital Health Ecosystem to become a Health Information Provider or Health Information User or efficiently link with building blocks of NDHM. The NS is, at its core, a formal programme for market participants to come forward to partner and integrate their current and new products, services, or business models with customers in a near-live environment, subject to certain safeguards and oversight.” ↑
- https://abdm.gov.in:8081/uploads/sandbox_guidelines_b39bcce23e.pdf, last accessed 07.01.2024 ↑
- https://samridhhealth.org/health-systems-design-webinar/, last accessed 03.01.2024 ↑
- https://ima-india.org/ima/pdfdata/IMA-Opinion-on-NDHM-Ecosystem.pdf, last accessed 04.01.2024 ↑
- Same as in Note 14 ↑
- Khoury and Ioannidis 2014. ↑
- https://www.pmindia.gov.in/en/news_updates/cabinet-gave-ex-post-facto-approval-on-the-memorandum-of-cooperation-between-india-and-bill-melinda-gates-foundation-bmgf-on-cooperation-in-the-field-of-health/ last accessed 03.01.2024 ↑
- https://www.gatesfoundation.org/our-work/places/india ↑
- https://www.gatesfoundation.org/about/committed-grants/2020/04/inv003040, last accessed 03.01.2024 ↑
- https://www.who.int/publications/i/item/9241800011
References
- Agarwal D, Roy N, Panwar V, Basil A, Agarwal PM. (2020) “Bringing health care closer to people – A review of various telemedicine models under the National Health Mission in India.” Indian Journal of Community Medicine 2020;45:274-7.
- Al Dahdah M and Mishra R (2020) “Smart Cards for All: Digitalisation of Universal Health Coverage in India.” Science, Technology & Society 25:3: 426–443. DOI: 10.1177/0971721820912920
- Bajpai, Nirupam; Wadhwa, Manisha (2021) “National Teleconsultation Service in India: eSanjeevani OPD.” ICT India Working Paper, No. 53, Columbia University, Earth Institute, Center for Sustainable Development (CSD), New York, NY. https://www.econstor.eu/bitstream/10419/249842/1/ICT-India-Working-Paper-53.pdf
- Balachandran M (2020) “Why the National Digital Health Mission could be a gamechanger”. Forbes India, August 28, 2020. https://www.forbesindia.com/article/healthcare-special/why-the-national-digital-health-mission-could-be-a-gamechanger/62071/1 Accessed on 31.12.2023
- Balsari S, Fortenko A, Blaya JA, Gropper A, Jayaram M, Matthan R, Sahasranam R, Shankar M, Sarbadhikari SN, Bierer BE, Mandl KD, Mehendale S, Khanna T. “Reimagining Health Data Exchange: An Application Programming Interface–Enabled Roadmap for India.” Journal of Medical Internet Research 2018; 20(7):e10725 doi: 10.2196/10725
- Bhavnani S P, Narula J, and Sengupta S P. “Mobile technology and the digitization of healthcare”. European Heart Journal (2016) 37, 1428–1438. doi:10.1093/eurheartj/ehv770
- Chakravarthi I, Hunter B M, Marathe S and Murray S. “Corporatisation in the private hospitals sector in India: case study from Maharashtra, India”. (2023) Economic and Political Weekly, vol 58 (11), pp 57-64.
- Chakravarthi I (2019) “Universal Health Care and Health Assurance through Healthcare Industry and Market Mechanisms: Evidence versus Ideology” in: Universalising Health Care in India: From Care to Coverage. Imrana Qadeer, K B Saxena, and P.M. Arathi (eds.) Aakar Books Delhi.
- Chaudhuri C and Datta P (2020) “Analysis of Private Healthcare Providers”. Economic & Political Weekly, October 31, 2020 vol 55 no 44, pp 59-64.
- CSDH (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, World Health Organization.
- Dhole K (2022) “Lessons from Digital India for the Right to Internet Access”. 25th ACM Conference On Computer-Supported Cooperative Work And Social Computing, Situating Network Infrastructure with People, Practices, and Beyond. November 8-22, 2022 (held virtually) https://arxiv.org/pdf/2211.06740.pdf. Last viewed January 1, 2024.
- Ecks S (2018) “‘When the Government Changes, the Card Will Also Change’: Questioning Identity in Biometric Smartcards for National Health Insurance (RSBY) in India.” Anthropologica, Vol. 60, No. 1, Thematic Section, pp. 190-200.
- Federation of Indian Chambers of Commerce and Industry (FICCI) and Boston Consulting Group (BCG) (2020) Leapfrogging to a Digital Healthcare System: Re-imagining Healthcare for Every Indian. https://web-assets.bcg.com/f6/3a/a701f7ab400494fe7aa600e96179/leapfrogging-to-a-digital-healthcare-system-bcg-ficci.pdf. Last viewed 5.2.2024
- Finley K. “Embattled Tech Companies Charge Deeper Into Health Care” (2018) WIRED March 1. https://www.wired.com/story/embattled-tech-companies-charge-deeper-into-health-care/ Last viewed February 5, 2024.
- Furtado K M, Raza A, Mathur D, Vaz N, Agrawal R and Shroff Z C (2022) “The trust and insurance models of healthcare purchasing in the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana in India: early findings from case studies of two states.” BMC Health Services Research 22:1056. https://doi.org/10.1186/s12913-022-08407-2
- Ganapathy K (2020) “Telemedicine in India: Personal Reminiscences from 1996.” TeleHealth Newsletter September 2020. https://tsitn.org/tsi-e-newsletter-sep2020/. Last viewed December 25, 2023.
- Ganapathy K (n.d.) “History of Telemedicine @ Apollo Hospitals India.” https://tsitn.org/history-of-telemedicine-apollo-hospitals-india/. Last viewed 25.12.23
- Government of India (2019) National Digital Health Blueprint. Ministry of Health and Family Welfare. Delhi.
- Government of India (2023) Report of the Comptroller and Auditor General of India on Performance Audit of Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana. Union Government (Civil) National Health Authority, Report No. 11 of 2023. Ministry of Health and Family Welfare, Delhi.
- Horton R. “Offline: Medicine and Marx” (2017) The Lancet Vol 390 November 4, p 2026.
- Hunter B M and Murray S F. (2019) “Deconstructing the Financialization of Healthcare.” 2019. Development and Change 0(0): 1–25. DOI: 10.1111/dech.12517
- Kanwar V, Chaudhary S, and Sharma A K. (2023) “Challenges in Implementing Digital Health Services in Rural India. The International Society for Telemedicine and eHealth 11, no. 1: 1-5.
- Khanduja P, Goli V and Singh S. (2021) “Reimagining the Indian government’s telemedicine platform.” https://www.microsave.net/2021/02/10/reimagining-the-indian-governments-telemedicine-platform/. Last viewed February 5, 2024.
- Khoury MJ, Ioannidis JP. “Big data meets public health” (2014) Science. November 28;346(6213):1054-5. doi: 10.1126/science.aaa2709.
- Kodali P B and Das S (2021) “Digital health technologies for universal health coverage: a promising change.” Current Science Vol. 120, No. 4, 25 February.
- Koh HC, Tan G. (2005) “Data mining applications in healthcare”. Journal of Healthcare Information Management. 19(2):64-72.
- Krishnan A, Nongkynrih B, Yadav K, Singh S, and Gupta V (2010) “Evaluation of computerized health management information system for primary health care in rural India.” BMC Health Services Research 2010, 10:310. http://www.biomedcentral.com/1472-6963/10/310
- Malhotra S (2023) “Cyberattacks hold up India’s push for digitisation of health.” British Medical Journal 2023; 380: p263. http://dx.doi.org/10.1136/bmj.p263.
- Mitra, A., Soman, B., Gaitonde, R., Bhatnagar, T., Nieuhas, E., Kumar, S. (2023). “Data Science Approaches to Public Health: Case Studies Using Routine Health Data from India.” in: Sharma, N., Goje, A., Chakrabarti, A., Bruckstein, A.M. (eds) Data Management, Analytics and Innovation. ICDMAI 2023. Lecture Notes in Networks and Systems, vol 662. Springer, Singapore. https://doi.org/10.1007/978-981-99-1414-2_63
- Naveen R Gowda N R, Satpathy S, Singh A R, and Behera S D. (2022) “The Holy Grail of healthcare analytics: what it takes to get there?” BMJ Leader 2022; 0:1–9. doi:10.1136/leader-2021-000527
- NITI Aayog, AIM, USAID, and IPE Global (2022) Reimagining Healthcare in India through Blended Finance.
- Pillutla R. “India’s digital mental health landscape: Government initiatives and challenges.” (2023) https://cmhlp.org/imho/blog/indias-digital-mental-health-landscape-government-initiatives-and-challenges/ Last viewed February 5, 2024.
- Prinja S, Bahuguna P, Gupta A, Nimesh R, Gupta M and Thakur J S. (2018) “Cost effectiveness of mHealth intervention by community health workers for reducing maternal and newborn mortality in rural Uttar Pradesh, India.” Cost Effectiveness and Resource Allocation 16:25. https://doi.org/10.1186/s12962-018-0110-2
- Ronquillo Y, Meyers A, Korvek SJ. (2023) Digital Health. in: StatPearls [Internet]: https://www.ncbi.nlm.nih.gov/books/NBK470260/
- Sarwal R; Prasad U; Madangopal K; Kalal S; Kaur D; Kumar A; Regy P; Sharma J.(2021) Investment Opportunities in India’s Healthcare Sector, NITI Aayog, March.
- Shao, Mingxing, Jing Fan, Zishan Huang, and Mingyang Chen. (2022) “The impact of information and communication technologies (ICTs) on health outcomes: A mediating effect analysis based on cross-national panel data.” Journal of Environmental and Public Health 2022.
- Sharma. R.S., Rohatgi, A., Jain, S., and Singh, S. (2023) “The Ayushman Bharat Digital Mission (ABDM): making of India’s Digital Health Story.” CSIT (April) 11(1):3–9. https://doi.org/10.1007/s40012-023-00375-0.
- Sieck C J, Sheon A, Ancker J S, Castek J, Callahan B and Siefer A (2021) “Digital inclusion as a social determinant of health.” npj/ Digital Medicine. 4:52. doi: 10.1038/s41746-021-00413-8
- Singh K P (2022) “Ransomware attack: Report flags host of security lapses at AIIMS.” Hindustan Times, December 7, 2022. https://www.hindustantimes.com/cities/delhi-news/report-flags-host-of-security-lapses-at-aiims-101670359251255.html
- Srivastava D (2015) “Health system monitoring using Health Management Information System (HMIS) in India and suggested enhancements to this platform.” International Journal of Scientific & Engineering Research, Volume 6, Issue 9, September.
- Srivastava S, Bertone MP, Parmar D, Walsh C, De Allegri M. (2023) “The genesis of the PM-JAY health insurance scheme in India: technical and political elements influencing a national reform towards universal health coverage.” Health Policy Plan. August 2;38(7):862-875. doi: 10.1093/heapol/czad045.
- Storeng K T. (2014) “The GAVI Alliance and the ‘Gates approach’ to health system strengthening.” Global Public Health, Vol. 9, No. 8, 865–879, http://dx.doi.org/10.1080/17441692.2014.940362
- United Nations (2012) Big data for development: challenges and opportunities.
- Vayena E, Salathé M, Madoff LC, Brownstein JS (2015) “Ethical Challenges of Big Data in Public Health.” PLoS Computational Biology 11(2): e1003904. doi:10.1371/journal.pcbi.1003904
- WHO-World Health Organization (2016) Global diffusion of eHealth: making universal health coverage achievable. Report of the third global survey on eHealth.
- Wyber, R., Vaillancourt, S., Perry, W., Mannava, P., Folaranmi, T., & Celi, L. A. (2015) “Big data in global health: improving health in low-and middle-income countries.” Bulletin of the World Health Organization, 93, 203-208. https://doi.org/10.2471/BLT.14.139022
- Zodpey SP, Negandhi HN. (2016) “Improving the quality and use of routine health data for decision-making.” Indian Journal of Public Health. 60:1-3. DOI: 10.4103/0019-557X.177248
↑